Diabetic Retinopathy
Vision loss due to diabetes affecting the performance of the retina.
Diabetic retinopathy refers to the changes that can occur in the retina in people with diabetes. The retina is the light-sensitive tissue at the back of the eye responsible for sending visual information up the optic nerve to the brain. In diabetic retinopathy, tiny vessels within the retina are damaged due to the effects of diabetes, if damage progresses it can lead to a reduced vision.
Who is at risk of diabetic retinopathy?
- All people with diabetes (Type 1, Type 2, & gestational diabetes).
- The risk of diabetic retinopathy is higher in people with poor control of diabetes, high blood pressure, high cholesterol, smokers.
What are the symptoms of diabetic retinopathy?
Some people with diabetic retinopathy can have normal vision. This is why it is important for all people with diabetes to have regular retinal checks. As diabetic retinopathy worsens it can lead to reduced vision. If this is severe and left untreated it can lead to blindness.
What are the types of diabetic retinopathy?
Non-Proliferative Diabetic Retinopathy (NDPR)
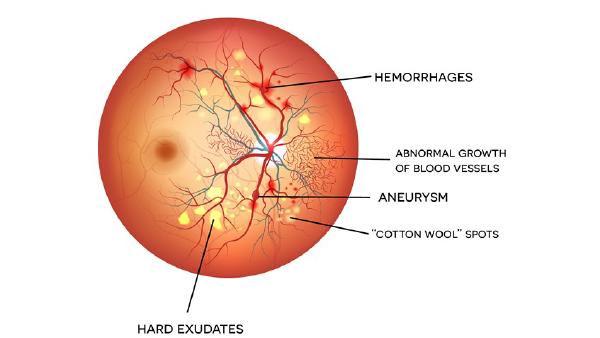
This is the early stage of the disease, where most people do not notice changes in their vision. As NPDR progresses, patients can develop retinal haemorrhages, leakage of fluid and fatty deposits in the retina. At this stage, it is important to aggressively try to prevent progression of the diabetic retinopathy. NPDR can lead to Proliferative Diabetic Retinopathy.Proliferative Diabetic Retinopathy (PDR)
As the disease progresses, areas of the retina lose their blood supply due to damaged retinal capillaries (small blood vessels). The eye attempts to re-supply the starving retina with oxygen but in doing so forms new, fragile blood vessels that can bleed easily.
In more advanced stages, frequent bleeds can cause scar tissue to form on top of retina. This pulls the retina out of position, causing a retinal detachment. In other cases, vessels can bleed into the vitreous causing a vitreous haemorrhage. This severely obstructs vision and can take weeks to months to be reabsorbed.
Retinal vessels that are damaged by diabetes can leak fluid and cause distortion of central vision. This is known as Diabetic Macular Oedema (DMO) and requires urgent treatment.
How can I prevent diabetic retinopathy?
The best way to prevent diabetic retinopathy would be by consulting with a GP, dietician and/or endocrinologist to achieve good blood sugar levels. In addition, ensuring blood pressure and cholesterol are well controlled is also important.
Early detection of diabetic retinopathy can significantly reduce the risk of blindness. For that reason, it is encouraged that people diagnosed with diabetes should have yearly check-ups.
What are the treatment options for diabetic retinopathy?
Intravitreal Anti-VEGF Injections
Anti-VEGF injections are used to treat Diabetic Macular Oedema (DMO). The medicine is injected into the eye to stop new blood vessel growth and leakage in the retina. In DMO there is an abnormally high level of Vascular Endothelial Growth Factor (VEGF) protein secreted by the abnormal retina. Anti-VEGF injections block this VEGF protein. The goal of treatment is to dry out the fluid between the retinal layers at the macula and lead to improvement of vision.Laser Photocoagulation
Pan-Retinal Photocoagulation (PRP) is a form of scatter laser that applies approximately 2,500 tiny burns on the peripheral retina away from the macula. These tiny burns shrink abnormal new blood vessels to reduce the risk of vision loss. More than one session of laser may be required. While preserving central vision, peripheral vision may be affected causing difficulty in low light. PRP works best before abnormal blood vessels start to bleed.
